Presented in part at the NICHD Conference, Research on Prevention of Bilirubin-Induced Brain Injury and Kernicterus-From Bench to Bedside, at Bethesda, Md, USA, June 2003.
Abstract
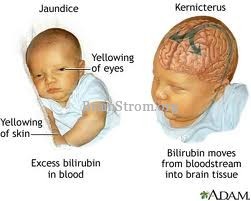
Kernicterus, thought to be due to severe hyperbilirubinemia, is an uncommon disorder with tragic consequences, especially when it affects healthy term and near-term infants. Early identification, prevention and treatment of severe hyperbilirubinemia should make kernicterus a preventable disease. However, national epidemiologic data are needed to monitor any preventive strategies. Recommendations are provided to obtain prospective data on the prevalence and incidence of severe hyperbilirubinemia and associate mortality and neurologic injury using standardized definitions, explore the clinical characteristics and root causes of kernicterus in children identified in the Kernicterus Pilot Registry, identify and test an indicator for population surveillance, validating systems-based approaches to the management of newborn jaundice, and explore the feasibility of using biologic or genetic markers to identify infants at risk for hyperbilirubinemia. Increased knowledge about the incidence and consequences of severe hyperbilirubinemia is essential to the planning, implementation and assessment of interventions to ensure that infants discharged as healthy from their birth hospitals have a safer transition to home, avoiding morbidity due to hyperbilirubinemia and other disorders.
At a recent NIHCD-sponsored conference, key questions were raised about kernicterus and the need for additional strategies for its prevention. These questions and an approach to their answers form the basis of this report.
A. IS KERNICTERUS A MATTER OF PUBLIC HEALTH CONCERN?
Available Evidence
Kernicterus has long been recognized as the pathologic sequela of severe hyperbilirubinemia. Although the condition is uncommon, the consequences are tragic, especially when it affects otherwise healthy term and near-term infants. Kernicterus has become uncommon because of effective screening for and prevention of Rh incompatibility, a historically important cause, and the accessibility of phototherapy to treat hyperbilirubinemia due to increased production and/or decreased elimination of bilirubin. Furthermore, adherence by clinicians to the guidelines from the American Academy of Pediatrics (AAP) concerning management of neonatal jaundice was expected to eliminate severe hyperbilirubinemia and prevent kernicterus.
Little contemporary information is available on the incidence or prevalence of kernicterus or its consequences. In the reports from the Pilot Kernicterus Registry and the Northern California Kaiser Permanente Medical Care Program (KPMCP) database, neonatal deaths due to kernicterus were ascertained from diagnostic codes on death certificates. Limitations of such observations include the retrospective design and possible under-reporting, delayed diagnosis, or errors in coding. For example, it is not feasible to estimate accurately a national incidence of kernicterus using the ICD-9 codes 773.4 and 747.7 for this diagnosis to query the HCUP database (Healthcare Cost and Utilization Project Agency for Healthcare Research and Quality, Rockville, MD; because the accuracy for annual reports is  70 cases. That kernicterus occurs is evident from 125 cases of infants who had been discharged as healthy from their birthing hospitals that were voluntarily reported from 1992 to 2002 to the Pilot Kernicterus Registry. In contrast, no cases of kernicterus in infants with cerebral palsy were found in the retrospective database of KPMCP during a similar time period (1991 to 1998). In addition, among these 111,009 infants in the KPMCP database, 11 (0.01%) developed total serum bilirubin (TSB) levels
70 cases. That kernicterus occurs is evident from 125 cases of infants who had been discharged as healthy from their birthing hospitals that were voluntarily reported from 1992 to 2002 to the Pilot Kernicterus Registry. In contrast, no cases of kernicterus in infants with cerebral palsy were found in the retrospective database of KPMCP during a similar time period (1991 to 1998). In addition, among these 111,009 infants in the KPMCP database, 11 (0.01%) developed total serum bilirubin (TSB) levels  30 mg/dl, and none of them apparently developed kernicterus. However, it is unclear whether all cases were identified, since TSB was not routinely measured in all infants nor were these infants followed prospectively.
30 mg/dl, and none of them apparently developed kernicterus. However, it is unclear whether all cases were identified, since TSB was not routinely measured in all infants nor were these infants followed prospectively.
The actual incidences of kernicterus or severe hyperbilirubinemia are not available because neither is a reportable condition. The incidence of severe hyperbilirubinemia has been estimated from a prospective study conducted in the 1960, a retrospective observational study of a population cared for in the 1990s, and additional prospective data from recent reports. Rates of readmission after the birth hospitalization range from 1.7 to 30.2 per 1000 live-births and represent a total of 42,470 readmissions for 1,532,924 live-births (27.7 per 1000) reported from 1988 to 1998.A disparity exists between term and near-term infants in the rates for readmission for jaundice. In a report of all California births from 1991 to 1999, C. Phibbs (personal communication) reported that near-term infants were consistently 6.4 to 6.6% of all well baby births (not admitted for neonatal intensive care), but their rate of readmission for treatment of jaundice was two- to three-fold higher than term infants
Figure 1.
 Rate of readmission for well babies for jaundice treatment in California (1991 to 1998) (California birth certificates were linked to the discharge abstracts for the birth hospitalization and readmission to identify the term and near-term well baby deliveries, and to separate readmissions for treatment of jaundice from those due to other causes.); data are presented for all well babies (
Rate of readmission for well babies for jaundice treatment in California (1991 to 1998) (California birth certificates were linked to the discharge abstracts for the birth hospitalization and readmission to identify the term and near-term well baby deliveries, and to separate readmissions for treatment of jaundice from those due to other causes.); data are presented for all well babies ( ) and separated as term (
) and separated as term ( ) and near-term infants (
) and near-term infants ( ).
).
Research Recommendation
Obtain data on prevalence, incidence, and mortality of severe hyperbilirubinemia and associated neurologic injury, including kernicterus.
B. WHAT IS THE RELATIONSHIP BETWEEN SEVERE HYPERBILIRUBINEMIA AND KERNICTERUS?
Available Evidence
A spectrum of neuronal injury associated with hyperbilirubinemia is known as bilirubin-induced neurologic dysfunction (BIND). The spectrum ranges from subtle or suspicious extrapyramidal or other manifestations to acute encephalopathy and chronic posticteric sequelae, although some of the signs are controversial.
Acute brain injury induced by bilirubin is associated with one or more posticteric sequelae in survivors. These are: (1) a movement disorder consisting of athetosis, dystonia, choreoathetosis, but also including spasticity and hypotonia, (2) auditory dysfunction consisting of deafness or hearing loss and auditory neuropathy or dys-synchrony, (3) oculomotor impairments, especially of upward gaze, and (4) dental enamel hypoplasia of the deciduous teeth.
Even though TSB is an important risk factor, bilirubin-induced brain injury and kernicterus cannot be defined on the basis of TSB alone. Factors including the albumin binding of bilirubin, hemolysis, gestational age, and genetic vulnerability modify the risk of kernicterus in an individual infant. However, there is a paucity of studies that evaluate the impact of these risk factors on the incidence of BIND or the occurrence of subtle sequelae or transient neurologic abnormalities.
Contemporary prospective population-based studies that describe the natural history of hyperbilirubinemia are unavailable; data are limited to studies before the advent of phototherapy. In addition, no prospective studies relate the incidence of kernicterus associated with specific TSB values.Thus, characterizing the risk of brain injury at specific levels of TSB is problematic. Furthermore, the safe level of TSB, below which BIND does not occur in otherwise healthy jaundiced infants, is not known. A standard definition of kernicterus in term and near-term infants is needed for purposes of research. This could include a threshold value for TSB, for example,  20 mg/dl, plus abnormalities of muscle tone on neurological examination, auditory neurophysiological testing, and magnetic resonance imaging.
20 mg/dl, plus abnormalities of muscle tone on neurological examination, auditory neurophysiological testing, and magnetic resonance imaging.
Research Recommendations
- Standardize definitions of severe hyperbilirubinemia, BIND, acute bilirubin encephalopathy, kernicterus. Uniform terminology is needed to compare databases and examine outcomes.
- Determine the prevalence and incidence of severe hyperbilirubinemia and kernicterus to estimate the risk of kernicterus at specific levels of TSB for term and near-term infants.
- Determine whether making a specific TSB level a reportable condition will accomplish this purpose.
- Develop a case–control study of adequate size to delineate the role of bilirubin and other factors in the development of kernicterus.
- Define population-based standards to help predict severe hyperbilirubinemia or, as important, the absence of risk based on predefined peak TSB levels.
C. WHAT ARE THE CHARACTERISTICS AND THE ROOT CAUSES OF RECENT CASES OF KERNICTERUS?
Preliminary Data
Preliminary data were presented on 125 of the 142 cases in the United States (including uniformed services) from the Pilot Kernicterus Registry (1992 to October 1, 2002). These infants were discharged as healthy and were included for analysis if they exhibited clinical signs of acute bilirubin encephalopathy and/or posticteric sequelae, regardless of TSB level and comorbidities. Most cases (about 50%) were voluntarily reported by parents or anonymously by physicians or nurses. One limitation of the registry is that these cases of kernicterus likely represent only a portion of affected children. Another limitation is that the population of newborns at risk because of severe hyperbilirubinemia is unknown, so that estimates of incidence and prevalence are unreliable. On the other hand, consistent observations from the registry provide the basis of recommendations for safe practices in order to prevent severe hyperbilirubinemia and kernicterus.
Characteristics of the population reported to the Pilot Kernicterus Registry (and individually listed in Appendix) included 84 male and 38 female cases, a racial distribution of White (58.4%), Black (26.4%), Hispanic (8.8%), Asian (6.4%) and the mean birth weight of 3281 g (range: 2015 to 4730). The mean gestational age was 38 weeks (range: 35 to 42.5). The etiology of hyperbilirubinemia in these infants, as evaluated upon readmission that was usually before 10 days of age, is listed in Table 3. All showed an excessive estimated rate of TSB rise (>0.20 mg/dl/hour) from birth to readmission. Analysis of these cases suggests the following root causes:(a) loss or lack of concern by clinicians regarding the neurotoxic potential of bilirubin, (b) limitations on visual recognition of jaundice as an index to initiate further evaluation or estimate severity, (c) failure to recognize the severity of hyperbilirubinemia at a specific age in hours; (d) failure to ensure appropriate follow-up 1 to 2 days after early discharge (24 to 72 hours of age); (e) delay in intensive or timely interventions before discharge or at readmission. More extensive analysis is needed of cases of kernicterus and predefined levels of severe hyperbilirubinemia (“close calls”) in order to better assess the performance of health-care providers and help address Institute of Medicine concerns, including patient (and family) centered care, quality of care, and patient safety.
Research Recommendations
- Conduct a comprehensive analysis of Registry cases to identify common characteristics, delineate the lapses in care that may have contributed to the occurrence of kernicterus, and determine the sentinel events that may have predicted the occurrence of kernicterus.
- Test the hypothesis that severe hyperbilirubinemia or kernicterus that affects babies discharged as healthy can be predicted before discharge.
- Assess the feasibility of a national reporting system and database for cases of pre-defined severe hyperbilirubinemia and kernicterus.
- Assess the feasibility of developing a systematic centralized review process, including root cause analysis, for prospective reported cases of severe hyperbilirubinemia that can be subsequently used to develop targeted education and systems improvements.
- Develop measurement tools to assess whether a centralized review process and interventions improve outcome.
D. WHAT SHOULD THE TARGET INDICATOR BE FOR PUBLIC HEALTH SURVEILLANCE OF KERNICTERUS AND/OR HYPERBILIRUBINEMIA?
At present, severe hyperbilirubinemia remains the most plausible surrogate indicator for kernicterus even though the risk of kernicterus at specific TSB ranges is estimated by clinical consensus rather than evidence-based criteria (Table 4). Surveillance for severe hyperbilirubinemia has distinct advantages. It describes an at-risk population, similar to identifying a population with hypertension regardless of its cause or its clinical outcome. TSB results are immediately available and objective, and can be reported rapidly. The inclusion of all cases, rather than just those with sequelae, would allow study of the risk of kernicterus in a population with hyperbilirubinemia, as well as study of the frequency and effects of any intervention. The TSB level at which cases might become reportable can be adjusted up or down based on risk and benefits. The immediacy and greater frequency of this outcome also make it potentially more useful for quality improvement efforts. Any initiative to begin surveillance for severe hyperbilirubinemia should be accompanied by efforts to improve standardization and minimize inter-laboratory variability.20
In general, there are at least four possible targets for public health surveillance related to kernicterus (Table 5). The first consideration is kernicterus itself. This disorder is the focus of current concern. However, the diagnosis may be delayed or under-reported. In addition, occurrences of kernicterus may be too infrequent (and too late) to provide feedback to health-care systems and providers that might reduce the risk of future cases. Surveillance for kernicterus would not capture other adverse effects of hyperbilirubinemia, including less typical sequelae and complications of exchange transfusion.
Like kernicterus, cerebral palsy is a highly relevant and clinically significant indicator. The diagnosis of cerebral palsy is already a matter of public health concern. Surveillance for cerebral palsy would allow studies of risk in children with different TSB levels, including those in whom TSB was never measured. However, the proportion of cerebral palsy due to kernicterus is not known, surveillance for cerebral palsy may be insensitive to changes in kernicterus incidence, and feedback to providers would be nonspecific and delayed.
Yet another surveillance strategy could be to monitor rates of readmission for treatment of hyperbilirubinemia or use of home phototherapy. Concomitant with incidence of severe hyperbilirubinemia, these offer useful indices of occurrence and outcome. On the other hand, interpretation is limited because intervention thresholds for severe hyperbilirubinemia have not been yet standardized.
Recommendations
- Identify an appropriate target indicator(s) for surveillance based upon advantages and disadvantages (Table 5).
E. HAVE SYSTEMS-BASED APPROACHES FOR THE MANAGEMENT OF NEWBORN JAUNDICE BEEN VALIDATED?
Available Evidence
Because of the concern for the reemergence of kernicterus,AAP and JCAHO recommend a universal systematic approach to the management of newborn jaundice, with the aim of reducing the incidence of severe hyperbilirubinemia and kernicterus. This involves using clinical risk factors analysis and/or measurement of predischarge TSB levels plotted an hour-specific nomogram to target appropriate follow-up and intervention. No prospective studies have compared or confirmed the effectiveness of such approaches. Whether a public health campaign to increase parental and provider awareness of jaundice and its potential consequences would reduce adverse outcomes is also unknown.
Research Recommendations
- Evaluate the recommendations for systems-based approaches for the prevention and management of severe hyperbilirubinemia. Approaches based on risk factors for severe hyperbilirubinemia or predischarge hour-specific TSB measurements should be prospectively validated for safety, costeffectiveness, and applicability to ethnically and racially diverse populations.
- Assess whether systematic prediction of severe neonatal hyperbilirubinemia prevents kernicterus in a cost-effective, practical and safe manner.
- Evaluate the epidemiologic impact of a public health campaign to reduce adverse outcomes of severe neonatal hyperbilirubinemia.
F. ARE THERE BIOLOGICAL OR GENETIC MARKERS THAT CAN BE USED TO BETTER DEFINE INFANTS AT RISK FOR SEVERE HYPERBILIRUBINEMIA?
Insufficient Evidence
The genetic contribution to neonatal hyperbilirubinemia due to disorders of hepatic bilirubin conjugation and to the pathogenesis of neuronal cell injury caused by hyperbilirubinemia needs further investigation.For example, early jaundice is greater in newborns homozygous for the polymorphism associated with Gilbert syndrome compared to those with the normal sequence or heterozygous for the mutation.The incidence of hyperbilirubinemia is also increased in infants who have the Gilbert polymorphism and glucose-6-phosphatase dehydrogenase (G6PD) deficiency. An investigation of microarray gene expression of hereditary disorders of unconjugated hyperbilirubinemia such as Gilbert, Arias, and Crigler-Najjar syndromes may elucidate possible coinheritance with G6PD deficiency, beta-thalassemia, and hereditary spherocytosis and identify infants at increased risk of severe hyperbilirubinemia. At this stage, it is too early to know whether genetic epidemiology of hyperbilirubinemia would contribute to the prevention of BIND.
Research Recommendation
Explore the feasibility of using diagnostic oligonucleotide microarrays for the known mutations of target genes to identify infants at increased risk of severe hyperbilirubinemia or those who have sustained kernicterus.
Infants discharged as healthy from their birth hospitals should have a safe transition to home, avoiding morbidity due to jaundice and other disorders. Prevention of readmission for severe hyperbilirubinemia in otherwise healthy infants, acute bilirubin encephalopathy, and chronic posticteric sequelae is a matter of public health and societal concern. Accurate data on the incidence of severe neonatal hyperbilirubinemia and associated adverse outcomes are fundamental to the planning, implementation, and assessment of interventions, including public policy and educational programs, to prevent adverse outcomes.
Thanks for installing the Bottom of every post plugin by Corey Salzano. Contact me if you need custom WordPress plugins or website design.