1. Talk too much
It’s not a conversation, and it’s not a debate. You are either treating their symptoms with medication, or guiding them to “treat” their own symptoms. Neither requires much talking.
If the psychiatrist says more words than the patient, then the psychiatrist is the patient.
Many psychiatrists talk because they feel powerless. The patient is in distress. How can the session be worth the money unless they get some thing? A prescription is good, but what else—what now? So the psychiatrist thinks they need to say something, to appear as though you are giving something to the patient. The worse the situation is, the more the psychiatrist talks. You’re talking to make yourself feel better, to justify your value as a psychiatrist. Don’t do this. It’s not help.
And empathize, don’t sympathize. I cringe whenever I see a psychiatrist on the first visit try to sound genuine while they affect a sad and shocked voice, lean forward, grab a box of tissues, “oh my God, I’m so sorry, that’s terrible!” It’s fake, which makes it annoying, but it’s patronizing, which makes it countertherapeutic. A psychiatrist cannot sympathize—did the same thing happen to you?. What they need to do is empathize, to understand the feelings, to appreciate them—not to share them. Plus, you don’t know what the situation means to the patient. Maybe they’re secretly happy (and guilty about it), and now that you’ve confirmed that it’s “terrible,” they’ll never admit to you or themselves they’re happy about it. Simply saying, “I’m sorry. Can you tell me more about…” is all that’s necessary.
And enough with the tissues. If you stalled the interview to go get them a box of tissues, you have failed, you changed the energy of a key moment. And you did this—let’s be honest—not because they needed tissues, but because it took some pressure off the moment and allowed you to give them something. Leave tissues by the patient chair from the beginning, and focus on what you’re doing.
I had a great mentor who taught me to begin the first session with the words, “Where would you like to begin?” And then to shut up. Great advice.
2. Take too much history
This is going to be controversial. I can hear academics seizing.
I know psychiatrists are taught that careful, meticulous history taking is the cornerstone of good care. Well, it’s not.
Every session should be about the patient, not about you. You’re supposed to help them, not understand them. The two may go together, but they might not. It is possible for you to help without understanding, but it is not acceptable for you to understand without helping. You’re not CSI, you’re not Batman, you’re not trying to solve a mystery or make some aha! discovery. They’re telling you what’s wrong. Just listen. Taking a detailed history may seem like a good idea, but many times it is masturbation, it contributes nothing to the patient’s well being, it only makes us feel thorough. As in: well, I can’t do much for him, but I got a really good history. Remember, it’s not about you, it’s about them. It may seem as if a strong family history of bipolar disorder is important information, but it isn’t. I know, bipolar runs in families and blah blah blah. You couldn’t tell they were bipolar before you learned their family history? And how do you know the family’s diagnosis was correct, so that you can rely on it to make your diagnosis?
I’m not saying don’t get the information. I am saying devoting the first one or two sessions exclusively to this gains the patient nothing. Everything from the moment they walk through the door should be about their service. Forget about the notes, especially outpatient notes. Worry about the patient, the notes should come second.
Are you proud of your notes because they contain so much detailed patient information? You need to think about this. Did you break eye contact to write, “sad over husband’s loss?” Then you missed the moment. Just listen—write your notes after the session. And if I see one more psychiatrist with a note pad playing stenographer I am going to punch him in the neck.
3. Ignore smoking cessation
or at least make it a secondary outcome. Also applies to soda/juice/calorie reduction.
This may seem trivial. It’s not—after the treatment of the initial presenting acute symptoms and treating drug and alcohol abuse, this is more important than almost anything in psychiatry. The logic is as follows:
1. Smoking is obviously and severely detrimental to one’s health, arguably more damaging than hypertension and depression combined. Its effect on life expectancy rivals, well, arsenic.
2. It is an addiction, so it is psychiatry’s business.
3. It is highly comorbid with psychiatric disorders, and may be a relative symptom of them. (For example: half of all people who commit suicide smoke.)
4. Smoking itself has a significant impact on other medications (e.g. did you know it reduces Haldol by half?)
5. What the hell else are you doing with the session? Especially in the “maintenance” phase of psychiatric treatment (where symptoms are relatively controlled, etc).
All of this applies equally to soda consumption or even diet in general. Drinking 2 liters of soda a day may not seem like a psychiatric issue, but most of the medications used have the propensity to increase appetite, and excess eating, smoking, soda drinking are hardly psychologically meaningless behaviors. If your psychiatrist asks you to keep a mood chart or teaches you about “serotonin dysfunction,” but doesn’t tell you to quit smoking, run. He has missed the forest for the trees.
4. Blame lawyers/insurance companies/Big Pharma
In order to understand why this is such a popular mistake among psychiatrists (all doctors, actually) it’s useful to identify when psychiatrists do this. There are two specific times. The first is when psychiatrists seek to justify doing, or not doing, some clinical maneuver, as in, “I can’t discharge him from the emergency room, even though I don’t really believe he is suicidal, I think he is lying simply to get hospitalized– but I don’t want to get sued.” The second time is when psychiatrists seek to explain a reduction in income, as in, “The insurance company only pays so much for a visit, so now I do only med checks.”
What is striking about these justifications is that they almost never relate to the specific problem at hand, they are scapegoats for some general anger about the difficulty of practice. For example, in the example of the malingering emergency room patient, discharging him has no increased risk of legal liability because if the patient is, in fact, malingering, then he will not kill himself. The operational issue here is not one of increased legal liability, but whether a physician can detect malingering. This has nothing to do with lawyers.
In the second example, while it is certainly true that the insurance company has set reimbursement rates, psychiatrists have not explored their responsibility in this. They have not, in any scientific, economic, and most importantly policy way, justified the necessity for a different (read: higher) reimbursement scheme. Consider psychiatrists’ attitudes towards psychologists acquiring prescribing privileges. It seems obvious that psychologists shouldn’t prescribe medications, but why not, exactly? To say that psychiatrists are trained in medicine and better understand drug-drug interactions, dosing, and toxicities presupposes that the average psychiatrist actually does know about drug-drug interactions, dosing and toxicities. Really? What’s the interaction between Prozac and hydralazine? Don’t know? Then why should psychologists know? And if you can look it up, so can they, etc, etc. Also, using this reasoning could backfire, as it can justify an insurance company refusing to pay for a psychiatric med check since the service could be performed by a primary care doctor (who will also handle everything else for the same low price.) Again, it is easy to complain, but it is on psychiatrists to explain, rationally, why it should not be.
Consider the common complaint that each insurance company has its own formulary, requiring doctors to prescribe alternatives, generics, or submit prior authorization requests. This is taken as bureaucratic interference of patient care. However, in the majority of the cases these restrictions are economically and clinically valid. No logic, let alone evidence, exists for prescribing two antipsychotics simultaneously. So why should the insurance allow it? Similarly, an insurance company should be allowed to approve drugs based on cost, because unless one can show that, for example, two SSRIs do not have the same general efficacy or tolerability across a population, than an insurance company cannot be reasonably obligated to provide both, especially if it can contract to receive one of the SSRIs at a cheaper cost. To be clear: it may, in fact, be true that (for example) two antipsychotics are better than one. But the burden of responsibility is on psychiatrists to show that this (or any clinical) maneuver is necessary, and not on the insurance companies to simply trust that doctors know best, because they have shown repeatedly that they do not.
Blaming lawyers has almost become a sport. It is certainly true that uncapped awards for damages hurts everyone (except lawyers.) However, lawyers are good at picking malpractice cases, not at inventing them. Consider informed consent: if one prescribes valproate for maintenance, one must not only discuss the side effects, but also the alternatives to treatment– especially when the alternatives to Depakote (a drug which has neither approval for maintenance nor rigorous data backing it) do have such approval and data (consider lithium, Zyprexa, Lamictal, etc.) To prescribe Depakote because it is at the top of an algorithm or in the “guidelines”, or because “that is my practice” and not because of a reasoned analysis of theindividual merits of the case, is at minimum not thoughtful practice. A similar example is psychiatry’s current obsession with antipsychotic induced diabetes. Assume that Geodon does indeed have a much lower risk of diabetes than Zyprexa; is a psychiatrist any less liable if the diabetes is induced by Geodon and not Zyprexa? No. You don’t get sued for using Zyprexa. You get sued for causing diabetes and never picking it up.
To state explicitly what seems the most obvious point of all: if a medication causes a side effect, and you catch it, there’s no lawsuit, because there’s no damage.
The above examples come from misunderstanding the available scientific literature, or not knowing it at all. Oddly, if a lawyer does not research the current state of case law and statutes before answering any legal question, it is legal malpractice. But doctors practicing medicine are not required to review current journal articles on any medical condition.
Pharma is the most maligned of all. On the one hand doctors resent the intrusion of the industry on their practice; on the other hand, industry is the primary—often only– ongoing educational source for doctors, whether they believe this or not. Drug reps, throwaway journals and supplements, “drug dinners” and almost all CMEs (yes, CMEs too, stop lying) are all industry sponsored educational processes which are the de facto continuing education of most psychiatrists. Oh, right, right– doctors learn by regularly reading numerous journals carefully and thoroughly. Ok–ask them to name one article in the most recent issue of the American Journal of Psychiatry. Not the results of the study; just the title.
One may want to ask why the FDA feels it necessary to hold pharmaceutical reps to extremely strict standards: they cannot mislead, they cannot speak off label, they must discuss side effects and toxicities, and they cannot use any promotional material that was not reviewed by the FDA. Used car salesmen are not held to any standards, and they sell to idiots. No one needs to tell you the rate of blowouts on a Firestone tire. Why would doctors—the most educated consumer group in existence—need protection from salespeople? Shouldn’t doctors, ultimately, know more about the medications than the sales reps do? Unless…
The sad truth is that the state of psychiatry is the fault of psychiatrists, who have failed to take full responsibility for their own education and practice. To blame anyone else at this stage is remarkably disingenuous.
5. Become social policy analysts
Remember how in May, 2005, the American Psychiatric Association endorsed same sex marriage? And you applauded the moral fortitude and progressive instinct of this august body? Well, instead of debating whether there should or should not be same-sex marriage, perhaps we should ask what modern psychiatry could possibly contribute to this discussion. The answer is nothing.
You can’t get away with pat answers, such as psychiatrists see the psychiatric ramifications of discrimination or being unable to marry. There are psychiatric ramifications of bankruptcy, and war, but no one felt compelled to write a policy statement on it (and thank God.)
And no, there isn’t a difference between bankruptcy and gay marriage– not to psychiatry. That’s the point. These are social problems about whichmodern psychiatry is definitionally ignorant. The APA did not endorse polygamy. What’s the difference? If homosexuality is not a psychiatric disorder, than there is no more reason to be more for or against it than there is for any other kind of marriage. The APA is no better suited to answering these questions than, say, the NFL.
What if the NFL came out against antidepressants in children? This is a perfectly valid analogy, because neither the NFL nor psychiatry have special knowledge that make their statements anything more than opinions. What do psychiatrists know about same-sex marriage that the quarterback for the Patriots doesn’t? Don’t laugh—I’m serious. What’s the answer?
Medicine, or the APA, can legitimately express a policy only if the policy was grounded in science or logic. Perhaps the APA cares to release this intriguing scientific data? (While it is at it, perhaps it can also release the data supporting the use of half of the medications currently favored by APA Guidelines?) But this seems pretty much business as usual for the APA. Rather than work on its own serious failings, it involves itself in social policy.
“Modern” (read: pharmacological) psychiatry is obsessed with reinventing itself as a biological and scientific discipline. Well, if it wants to be a science, it better start acting like one.
The FDA effectively killed Vioxx, and not a peep was heard from the APA about the dangers of letting the government regulate their practice. You can say Vioxx has little to do with psychiatry, but it’s still a lot more than gay marriage.
Determining what is true and what is not, through serious and often disconcerting scientific enquiry, is very difficult. It is much easier to involve oneself in matters of opinion and debate, in activism, because it is both immediately rewarding and it is easy. It’s hard to measure things in psychiatry, and when it is possible the results are often disappointing. So it busies itself with matters of conviction because it feels some responsibility to have convictions. It doesn’t. It has a responsibility to the truth, and if it doesn’t want to invest any energy in that pursuit, it is on them. But don’t mask it with whimsy and dilettantism.
I should point out that gays, far from being pleased with the APA’s stand, should actually be horrified. Do you– does anyone– want social policy suggested by psychiatrists? Think long and hard.
Imagine the outrage if the APA had come out against gay marriage, or forthe war in Iraq. There would be battalions of people saying, “well, what the hell do psychiatrists know about war in Iraq? Who the hell do they think they are telling gays not to get married?” There is no protection in being confident of the rightness of your current position, as history is loaded with examples of how terribly bad doctors are at determining what is right and what is wrong. Not long ago homosexuality was considered a disease. See? The Tuskegee experiments were endorsed by the AMA, and the AMA gave its endorsement, after ethics concerns were raised by Peter Buxtun. Remember that? How about the speech to the1941 APA meeting, and the1942 issue of the American Journal of Psychiatry in which euthanizing the “feebleminded” (IQ<65) sounded like a good idea?
Psychiatry would do well to remember Wittgenstein TLP 7: Whereof one cannot speak, thereof one must be silent.
6. Don’t refer to therapy.
Psychopharmacology without therapy is treating an infection with Tylenol.
Medications do not cure a psychiatric disease; we’re not even sure what the disease actually is. What they can do is reduce symptoms, give you strength—so that you can learn new behaviors. That’s the point of medications. Treating depression with an antidepressant is not the solution; it’s the preliminary step in allowing you to figure out how to handle depression later on. The adaptation, the adjustment, the physical altering of brain functioning is done by new learning, often this is therapy (though it doesn’t have to be.) I’m not saying therapy is that great, or necessary, either. I’m simply saying that trying to improve a person’s long term status using medications alone without some sort of education and training is a waste of time. It is maybe the most profound disservice of all to tell a patient that their depressive or bipolar symptoms are the result of biology or chemical imbalances and thus absolve them of the responsibility of learning new ways of interpreting and coping with their environment.
7. Don’t think strategically.
Psychiatry is fun, I’m sure, but it doesn’t help anybody when the patient refuses to play. Psychiatry telling us opiate abuse is a heritable disorder related to polymorphisms in dopamine receptors doesn’t stop your kid from stealing your money to buy smack. See? Sometimes you have to hide your wallet.
What is the goal? What do you have to do to achieve that goal? Sometimes you have to look beyond the DSM.
Do what you have to do. When a person needs treatment but is refusing it, neither the law nor psychiatry can help them. I can’t force someone into treatment. But you can. Take drug abuse: in my experience, the only way to get someone to (albeit reluctantly) accept treatment is a large scale intervention. 10 people, minimum, in a cramped room with the future patient trapped as far form the door as possible, all ten in energetic agreement that the person needs to get help– now. Not tomorrow morning. Immediately. You’ve already packed his bags. This isn’t a five minute pep-talk—take the whole day off, you’re going to be there a while. Also, a psychiatrist cannot do this for you, he shouldn’t even be there, because no one ever listens to neutral third parties, much less psychiatrists. (And I’ll just say it: you probably don’t want a psychiatrist there in case you…have to take things… to the next level…) It has to be ten highly motivated, concerned people. If you are not motivated enough to stage this uncomfortable intervention, I assure you he won’t be motivated to go. This is the kind of thing a psychiatrist should be telling you, not trying to sell you on Suboxone. Nobody likes confrontation or to be confronted. Ten people. Minimum. Sure, you are partly guilting them into treatment, partly coercing. But getting them into treatment in this way is better than not getting them into treatment in a nicer way. Psychiatry is war.
Sometimes people don’t need to know. If a person’s life is changed on medication, it may be okay not to tell them all the side effects. I know, lawyers are standing by (see # (blame lawyers), but again, it’s strategy, and I think reasonable people (i.e. juries) will understand what you were doing. If lithium keeps the person from slitting their own throat, it’s okay to skip the part about how it can hurt your thyroid. It doesn’t exempt the doctor from checking for it, mind you. In these tricky situations, a) you have to be sure this medication is absolutely vital; b) recruit as many people as possible into the therapeutic umbrella. Tell the wife about the side effect; tell family what to watch out for. And monitor. There’s even a technical term for this therapeutic privilege, but I can’t remember what it was.
Save the environment. Here’s an all too common scenario involving no strategic thinking: Your adult child is living at home, no job, sporadic drug use, involved in an abusive relationship, frequent quasi-suicidal acts, etc. You’ve tried everything, nothing has worked. You don’t know what to do. You’re afraid to kick them out because they can’t manage on their own, you’re afraid they’d sink deeper into drugs/depression/etc; but on the other hand you have other kids you have to worry about, a finite supply of money, etc, etc. You’re paralyzed.
Here’s a question you might not have thought about: what happens to the kid when you die? They are suddenly going to be without support, suddenly without money, suddenly without resources. Will they simply manipulate your spouse into getting their needs met? Or worse, go somewhere else? Is that what you want? Plan today, now, for this eventuality. Maybe that means setting up a trust with a finite monthly payout only if they are living on their own and have a paycheck. Or only if they are seeing a therapist once a week. Or give clean urines. “What is this, probation?” Actually, that’s exactly what it is.
You have to save the environment you are in before you can help the other person. That means protecting your wife and other kids, and their physical assets. It means protecting your marriage. It may seem cold to worry about money when your kid’s on heroin, but I assure you that this is the most important thing you can do if the kid won’t get help. Ripping apart your marriage over this benefits no one, absolutely no one. So yes, it may mean kicking them out of the house, cutting them off. It also means doing an intervention. It means holding your breath that that phone is going to ring in the middle of the night and it’s going to be the police. But letting them eat, sleep, and watch TV in your house while their chaos continues does not lessen the risk of receiving that phone call.
It’s called enabling. Don’t do it. And a psychiatrist should be telling you this, not trying to give you Celexa to help you cope with it.
8. Polypharmacy
Polypharmacy isn’t just common– it’s the codified standard. When two psychiatrists discuss a patient, inevitably one of them will say these four words: “You should consider adding…”
The paradigm is that if you fail a medication, you must be so sick that you need a second medication.
It’s a useful paradigm; and by useful, of course, I mean wrong. Here’s an alternative paradigm: maybe if the medication didn’t work, you should try a different one?
Polypharmacy would be ok if there was at least some data justifying it. But there isn’t. I know, controversial. Look it up.
Consider antipsychotics: if anyone can provide the logic– not data, simply the logic– for using two simultaneously, I’d love to hear it. Antipsychotics work by blocking dopamine receptors, of which there are supposedly a finite number. If one antipsychotic blocks most of them, where is the other supposed to go? Why couldn’t you simply increase the dose of the first? And if side effects prevent this increase, why wouldn’t you just switch to the second medication?
Same with antidepressants: Zoloft and Prozac are SSRIs, they target the exact same molecule, which is again finite in number. If most are blocked by one drug, where does the second go? Why are you offended that Medicaid doesn’t let you prescribe two at the same time?
So you say: well, what about mixing two drugs of differing pharmacologies, like Zoloft (serotonin) and Wellbutrin (dopamine/norepinephrine)? At least there is logic to this one, but–surprise- no evidence. It may seem as though Zoloft + Wellbutrin, or Depakote + an antipsychotic, etc is better than one alone, but they’re not. But here’s the point: even if it were true, so what? How do you know it’s necessary? Shouldn’t prudence and common sense and fiscal responsibility and the cramp in your writing hand require you to at least try monotherapy a few times? Twice, at least? Because I can’t prove two drugs are better than one, but I can prove they are twice as toxic and twice as expensive.
Polypharmacy is bastard child of the theory of maintenance treatment. If it took three medications to get you feeling better, then you need to continue these three medications in order to stay stable. Going off your medications results in disaster.
First of all, no. Secondly, take the example of mania. If you’re manic, and it took three medications to bring the mania down, does that mean you need those three for the rest of your life? Because if so, what do you do the next time you get manic? Add a fourth? Don’t you get used to medications? Does tolerance not occur? Upregulation and all that? You see the problem– maintenance begats polypharmacy. Also, medications have side effects, and so medications are given for the side effects of the other
medications, ad nauseum. At some point (four medications?) the symptoms you are seeing cannot be reliably ascribed to the disorder rather than the medications themselves. The patient is buried. The treatment now becomes getting them off these medications.
Again: it may be true that an individual person needs several medications. But you can’t make polypharmacy a generalized treatment standard. It’s too expensive and has too many side effects for a theoretical benefit. And what kind of message does it send to the patient? If you’re on four medications, how can you be anything but severely ill, all the time? How can you be responsible for any of your feelings, or for controlling them?
9. Diagnose everything
The layman’s argument is that psychiatry pathologizes everything: “well, anyone would be depressed in those circumstances. How is that an illness? And why can you get SSI for it?”
But the truth is in the nuances. When psychiatrists ask you to keep a mood chart, and you report that on these two days your “depression was worse,” what allows the psychiatrist to know that wasn’t normal sadness? Can a bipolar ever be sad for a month and not be depressed?
If a person beats his girlfriends, kills cats, and gets brought by the police because he set fire to a rival’s car, is it possible that his Axis I diagnosis is—nothing? Ok—how many times have you actually written that down? How many times have you terminated the “treatment,” or refused to uphold an involuntary commitment order, because the case was not psychiatric? I know, the system does not have a good mechanism for doing this. I feel your pain. But every time we give some vague “Not Otherwise Specified” diagnosis or pass them along to the inpatient services, we are creating a social policy disaster. We are confirming to the laymen that we think these behaviors are psychiatric, that they are rightfully our purview, and ensuring that a) we will be held responsible for dealing with them; b) we will be held responsible for the outcome.
Thanks for installing the Bottom of every post plugin by Corey Salzano. Contact me if you need custom WordPress plugins or website design.








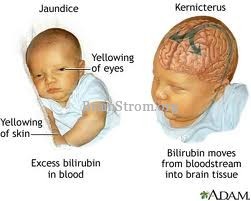
 70 cases. That kernicterus occurs is evident from 125 cases of infants who had been discharged as healthy from their birthing hospitals that were voluntarily reported from 1992 to 2002 to the Pilot Kernicterus Registry. In contrast, no cases of kernicterus in infants with cerebral palsy were found in the retrospective database of KPMCP during a similar time period (1991 to 1998). In addition, among these 111,009 infants in the KPMCP database, 11 (0.01%) developed total serum bilirubin (TSB) levels
70 cases. That kernicterus occurs is evident from 125 cases of infants who had been discharged as healthy from their birthing hospitals that were voluntarily reported from 1992 to 2002 to the Pilot Kernicterus Registry. In contrast, no cases of kernicterus in infants with cerebral palsy were found in the retrospective database of KPMCP during a similar time period (1991 to 1998). In addition, among these 111,009 infants in the KPMCP database, 11 (0.01%) developed total serum bilirubin (TSB) levels 
