Modifications of lipoinjection techniques to improve the survival rate for injected fat have been attempted. From these, it is well accepted that adipose tissue should be placed as small aliquots [
3], preferably within an area 3 mm in diameter [
1]. Because it takes a long time to perform ideally diffuse distribution of suctioned fat [
3], we have used a disposable syringe with a threaded plunger and connections, a very long needle (150 mm), and an assistant to rotate the plunger. As a result, only 35 to 60 min are required for injection in both breasts. These devices are critical to performing large-volume lipoinjection safely and precisely in a short time.
In addition, the harvesting, preserving, and refining of graft materials also are important, as repeatedly indicated in the literature. We used a relatively large suction cannula, centrifuged the aspirated fat in some cases, and kept it cooled until transplantation. In this study, the clinical results (increase in breast circumference) appeared to be better in group C (using centrifuged fat) than in group A (using noncentrifuged fat), although quantitative measurement and statistical comparison were not done. In a previous study, we found that centrifugation of aspirated fat is substantially influential because centrifugation at 1,200 g decreases the fat volume by 30%, damaging 12% of the adipocytes and 0% of the ASCs. This leads to the concentration of cell numbers per volume of adipocytes and ASCs by 25% and 43%, respectively [
7].
In addition, centrifugation may be especially beneficial in our treatment because water content in the graft material may disturb the adherence of ASCs to the adipose tissue and interfere with differentiation into expected lineages. Any ASCs floating in a solution, which is a nonphysiologic environment, may migrate over distances, penetrate into the lymphatic flow, and differentiate unexpectedly. We believe that such migration and altered cell differentiation caused the development of fibrotic tissue on the sternum of one patient in group B. Thus, we conclude that centrifuged fat combined with ASCs as cell pellets (group C procedure) was best among the three methods used in this study.
Although small cystic formation and microcalcification were detected in some cases, the microcalcification was easily distinguished from that associated with breast cancer, and the overall cosmetic results were generally satisfactory and encouraging. Almost all the patients were satisfied with their enlarged and soft breasts with a natural contour. Both CT scans and MRI showed that transplanted fat tissue survived and formed a significant thickness of the fatty layer not only subcutaneously on and around the mammary glands, but also between the mammary glands and the pectoralis muscles. Breast volume stabilized 2 to 3 months after transplantation.
Maximum breast augmentation using the described technique varied among the patients and appeared to be 100 to 200 ml. Although these volumes may be smaller than those achieved with large artificial implants, a definite advantage is that patients need not be concerned about postoperative complications induced by artificial implants such as rupture, infection, capsular contracture, unnatural contour, hardness, neurologic symptoms, and immune response. Compared with our dozens of patients who underwent conventional autologous lipoinjection to the breasts, augmentation effects were apparently higher with CAL. A 2- to 3-cm increase in breast circumference was common with the conventional procedure, compared with the 4- to 8-cm increase seen in this trial of CAL, although the augmentation effect varied among patients. The measurement system we recently devised may help to quantify the difference in augmented volume in the future.
Adipose tissue contains not only adipogenic progenitor cells, but also multipotent stem cells, which can differentiate into fat, bone, cartilage, and types of tissue [
21,
22]. Suctioned fat appears to lose a significant number of these precursors during liposuction and the preparation processes as compared with nonsuctioned adipose tissue [
9]. This relative deficiency of precursors may contribute to the low survival rate and long-term atrophy of transplanted lipoaspirates. In CAL, the deficit of ASCs was compensated by supplementing ASCs. To maximize the biologic function and avoid unexpected behavior of ASCs, it seems important to ensure adherence of supplemented ASCs to adipocytes or connective tissue.
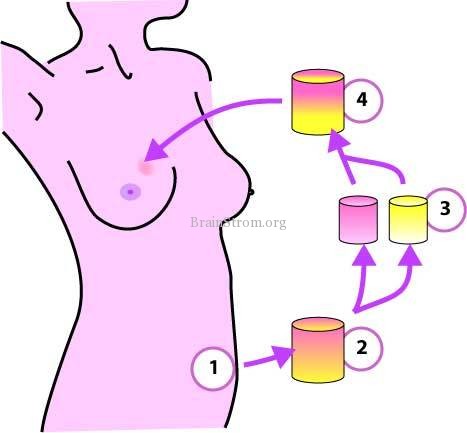
With this novel treatment, ASCs have four possible roles, which were partly confirmed in preclinical studies [
8,
9,
11]. First, ASCs can differentiate into adipocytes and contribute to the regeneration of adipose tissue. Second, ASCs can differentiate into endothelial cells and also probably into vascular mural cells [
8,
10,
12], resulting in the promotion of angiogenesis and graft survival. Third, ASCs are known to release angiogenic growth factors in response to hypoxia and other conditions [
13], and these factors influence surrounding host tissue. In their final role, which may be the most influential, ASCs survive as original ASCs [
9]. In the adipose tissue, ASCs reside between adipocytes or in the extracellular matrix, especially around vessels, and contribute to the turnover of adipose tissue, which is known to be very slow (2 years or more) [
17]. However, adipose grafts probably turn over during the first 2 to 3 months after transplantation because they experience temporary ischemia followed by reperfusion injury. This turnover, the replacement process of the adipose tissue, is conducted by tissue-specific progenitor cells, which are ASCs. The relative deficiency of ASCs in aspirated fat may affect the replacement process and lead to postoperative atrophy of grafted fat, which is known to occur commonly during the first 6 months after lipoinjection.
The freshly isolated SVF used in CAL contains not only ASCs but also vascular endothelial cells, pericytes, blood cells (both white and red), and other cells, as previously described [
20]. After transplantation, ASCs may interact with other cells such as vascular endothelial cells, and supplementation with the SVF may be superior to supplementation with ASCs alone in this treatment. However, further studies are needed to elucidate the synergistic effects of ASCs with other cells contained in the graft.
In this preliminary study, satisfactory clinical results were generally achieved without any major complications. Thus, we can conclude that CAL is sufficiently safe for continuation of the study, though controlled investigations and accumulated long-term results are needed to elucidate the overall safety and efficacy of the treatment. A variety of new innovations, including stem cell technology, may be developed and may contribute to the improvement of autologous tissue transplantation and regeneration. Further improvements of the technique may cause autologous tissue transfer to become the first choice for breast augmentation in the future.
 1 Katsujiro Sato,2 Noriyuki Aoi,1 Masakazu Kurita,3Toshitsugu Hirohi,4 and Kiyonori Harii3
1 Katsujiro Sato,2 Noriyuki Aoi,1 Masakazu Kurita,3Toshitsugu Hirohi,4 and Kiyonori Harii3 Corresponding author.
Corresponding author. This article has been cited by other articles in PMC.
This article has been cited by other articles in PMC.